How to measure prostate volume without ultrasound
If you’re wondering how to measure prostate volume without ultrasound, you’re not alone. Many men want to understand their prostate size, but don’t always have access to ultrasound scans.
Fortunately, there are reliable alternatives—from MRI or CT imaging formulas to PSA-based estimates and even clinical exam grading—that can give you a clear idea of your prostate volume.
In this guide, you’ll discover each method step by step, helping you know which option fits your situation best and why it matters for your health.
The two main methods for estimating prostate volume without ultrasound are:
- Digital Rectal Examination (DRE): This is the most common and traditional method. A trained healthcare provider uses a gloved, lubricated finger to feel the prostate gland through the wall of the rectum.
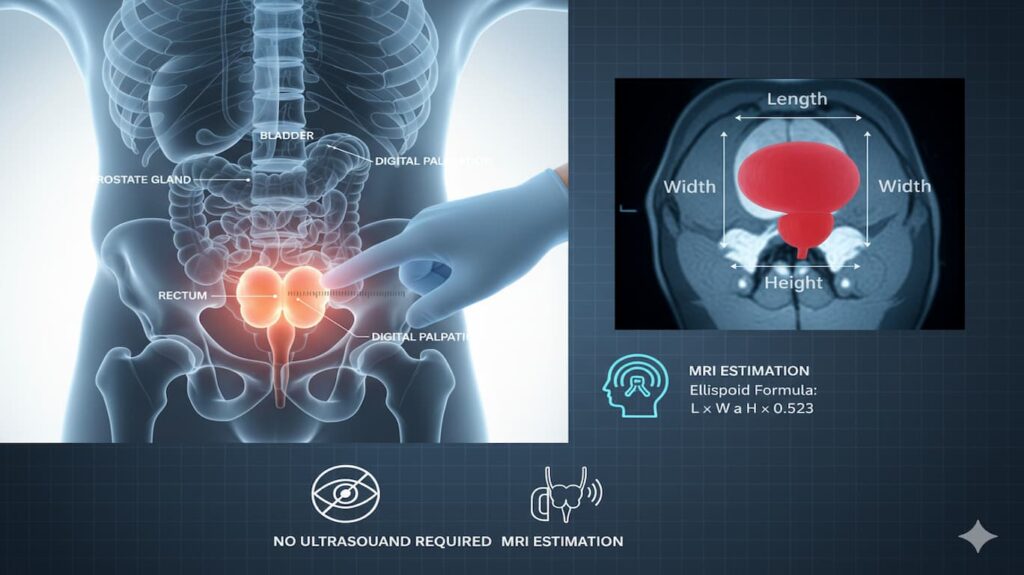
- Magnetic Resonance Imaging (MRI): While a powerful imaging tool, MRI is a “non-ultrasound” method for prostate measurement. It provides a highly detailed and accurate measurement of the prostate and is often used when a more precise assessment is needed, or to look for other abnormalities. However, it is more expensive and not a routine part of a general check-up.
Here are the practical ways clinicians estimate prostate volume without ultrasound—plus exactly how you can do the math yourself when you have the right numbers.
I’ll give you three routes (from most to least accurate), with worked examples and what to watch out for.
1) From an MRI or CT report (most accurate without ultrasound)
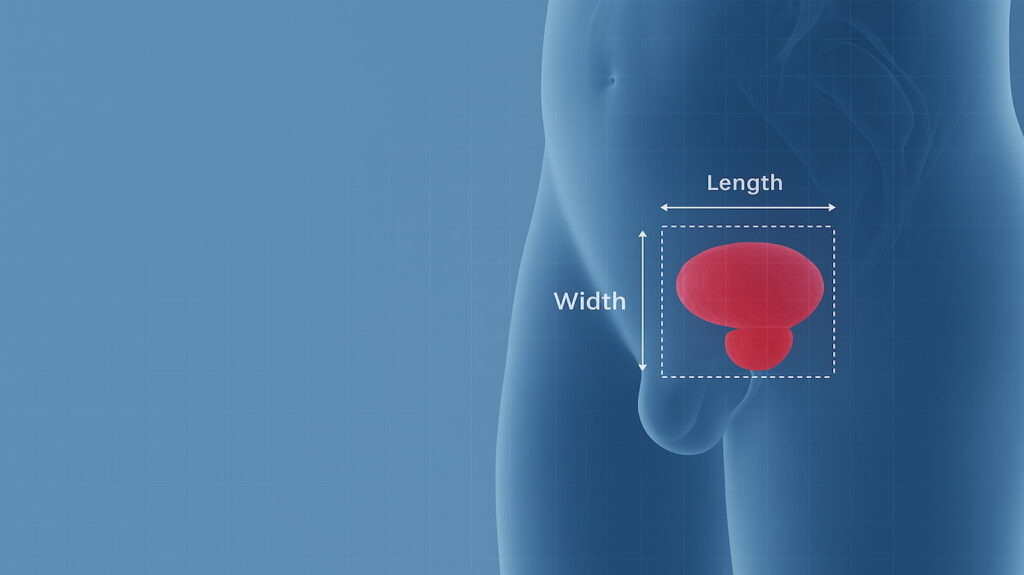
Most radiology reports list either the prostate volume outright or the three linear dimensions:
- Length (cranio-caudal)
- Width (transverse/left-right)
- Height (antero-posterior)
If you see only the three dimensions, calculate volume using the standard ellipsoid formula:
Prostate volume (mL or cc) = Length × Width × Height × 0.52
- Units must be centimeters.
- If your report already lists “prostate volume,” you can use it directly.
✅ Example
Report shows AP (height) 3.8 cm, TR (width) 4.7 cm, CC (length) 3.6 cm.
Volume ≈ 3.6 × 4.7 × 3.8 × 0.52 = ~33.4 cc.
Why this works: the prostate is roughly ellipsoid, and MRI/CT dimensions plugged into the ellipsoid formula are widely accepted in radiology and urology practice.
Note: Some papers propose alternative coefficients (“bullet” model ~0.65–0.66) to slightly improve accuracy, but 0.52 remains the standard and is what most clinical tools use.
2) From a clinician’s DRE (digital rectal exam) note (rough clinical estimate)
If your clinic notes include a DRE grade for benign prostatic hyperplasia (BPH), you can translate that to an approximate volume range:
- Grade I → ~28 mL (± ~3)
- Grade II → ~41 mL (± ~8)
- Grade III → ~61 mL (± ~12)
- Grade IV → ~98 mL (± ~23)
(Clinicians often also summarize as: Grade I <30 mL, Grade II 30–50 mL, Grade III 50–85 mL, Grade IV >85 mL.) Because prostate tissue density is ~1 g/mL, grams ≈ mL.
Important safety note: Don’t attempt a self-DRE. It’s invasive, can cause injury/infection, and requires training. If you have a clinician’s DRE note, use the mapping above; otherwise, stick to MRI/CT or the PSA-based estimate below.
3) From a PSA blood test (very rough, for ballpark only)
If imaging isn’t available, you can make a coarse estimate using PSA density (PSAD) concepts. PSAD = PSA / Prostate Volume. Rearranged:
Estimated prostate volume ≈ PSA / Assumed PSAD
Clinically discussed PSAD cut-points (used for risk triage, not measurement) are commonly 0.15 ng/mL/cc, with growing support for ≥0.20 ng/mL/cc as a stricter threshold. You can use those as assumptions to form a range:
- Using 0.15: Volume ≈ PSA ÷ 0.15 (= 6.7 × PSA)
- Using 0.20: Volume ≈ PSA ÷ 0.20 (= 5 × PSA)
✅ Example
If PSA = 6.0 ng/mL
• Assuming 0.15 → ~40 cc
• Assuming 0.20 → ~30 cc
So you might quote a rough range 30–40 cc.
Caveats: PSA rises with prostatitis, urinary retention, recent ejaculation, cycling, and varies with medications (e.g., finasteride halves PSA). This method is crude and should not be used to diagnose or rule out cancer—just to get a ballpark size when nothing else is available.
Quick checklist (pick what you have)
- MRI or CT report in hand?
→ Read off volume if given. If not, take Length, Width, Height (cm) and compute L×W×H×0.52. - Clinic note with a DRE grade (I–IV)?
→ Map to the ranges above (e.g., Grade II ≈ 30–50 mL). (Lippincott Journals) - Only a PSA value?
→ Estimate “ballpark” volume using PSA/0.15 and PSA/0.20 to create a range, and treat it cautiously. (PMC)
What’s “normal” size?
Typical adult prostate volume is roughly 20–30 cc (≈ grams). Individual variation is large and size doesn’t perfectly track symptoms.
How to Use a Prostate Volume Calculator
Our prostate volume calculator above requires three simple measurements (usually from a transrectal ultrasound (TRUS) or MRI):
- Length (cm) – Longest axis
- Width (cm) – Side-to-side measurement
- Height (cm) – Front-to-back measurement
Enter these values, and the calculator will provide:
✔ Prostate volume (cm³)
✔ Estimated weight (grams)
Example Calculation:
If a prostate measures 4.0 cm (length) × 3.5 cm (width) × 3.0 cm (height):Volume=π6×4.0×3.5×3.0≈22.0 cm³Volume=6π×4.0×3.5×3.0≈22.0cm³
This suggests a mildly enlarged prostate (normal range: 20-30 cm³).
Prostate Volume Calculator
This tool estimates prostate volume (in cm³) using the ellipsoid formula (length × width × height × π/6), the standard method for ultrasound or MRI measurements.
Volume is converted to weight (grams) assuming a tissue density of 1.05 g/cm³. Useful for clinical assessment of benign prostatic hyperplasia (BPH) or prostate cancer monitoring.
🔬 Prostate Volume Calculator
Calculate prostate volume using ultrasound measurements
This uses the ellipsoid formula with correction factor commonly used in medical practice
Accuracy notes & tips
- MRI/CT ellipsoid is your best non-ultrasound option and is acceptable for clinical use. (PMC)
- DRE gives only a rough size band and depends on examiner skill. (Lippincott Journals)
- PSA-based estimates are ballpark only and easily skewed by inflammation, infections, recent ejaculation, catheters, or medications; use as a range, not a single number.
Step-by-Step Guide for Digital Rectal Examination (DRE) for Prostate Volume Estimation
Important Note: This is a procedure that must be performed by a qualified medical professional. It is not something you can do yourself, and this guide is for informational purposes only to help you understand the process.
1. Preparation: * Patient Positioning: The patient is typically asked to lie on their left side with their knees bent towards their chest (fetal position) or to stand and bend forward at the waist.
* Bladder Emptying: The patient should empty their bladder before the examination, as a full bladder can make the prostate feel larger than it is.
* Lubrication: The healthcare provider will wear a lubricated glove on their finger to ensure comfort and ease of insertion.
2. The Examination:
* The healthcare provider will gently insert their index finger into the patient’s rectum.
* They will then palpate (feel) the posterior surface of the prostate gland. The prostate is located in front of the rectum, below the bladder, and it surrounds the urethra.
* The provider will systematically feel the entire gland, noting its size, shape, symmetry, consistency, and any irregularities or nodules.
3. Estimation of Volume: * DRE is a subjective method and relies on the physician’s experience.
* Instead of giving an exact volume in cubic centimeters (cc) or milliliters (mL), the provider will often use a grading system to estimate the size. A common system uses a comparison to familiar objects:
* Grade 1 (Slight enlargement): Roughly the size of a chestnut, protruding slightly into the rectum. This corresponds to a volume of approximately 25-30 cc.
* Grade 2 (Moderate enlargement): About the size of a plum, filling less than half of the rectal lumen. This is often associated with a volume of around 50 cc.
* Grade 3 (Significant enlargement): The size of a lemon or orange, filling more than half of the rectal diameter. This corresponds to a volume of 75 cc or more.
* Grade 4 (Marked enlargement): The prostate is very large, possibly the size of a grapefruit, and the examiner may have difficulty reaching its upper limits. This can be over 100 cc.
4. DRE Limitations: * DRE is highly dependent on the examiner’s skill and experience.
* It can underestimate the size of the prostate, especially for larger prostates or when the enlargement protrudes into the bladder rather than the rectum.
* It only allows for the examination of the posterior portion of the gland.
* The size estimation is an approximation, not a precise measurement.
5. Other Non-Ultrasound Methods
- Magnetic Resonance Imaging (MRI): A more accurate method than DRE. MRI provides detailed images of the prostate from which dimensions can be measured. The volume is then calculated using the ellipsoid formula.
-
- Ellipsoid Formula: The most common formula for calculating prostate volume from dimensions is: V=L×W×H×6π≈L×W×H×0.523 Where L is length (craniocaudal), W is width (transverse), and H is height (anteroposterior).
- These dimensions are measured directly from the MRI images.
- MRI is used to get a precise measurement, especially for treatment planning for conditions like prostate cancer or benign prostatic hyperplasia (BPH).
Conclusion on how to measure prostate volume without ultrasound
While you cannot measure your own prostate volume, a healthcare provider can estimate it using a digital rectal examination (DRE).
This is a quick and simple initial assessment that provides a rough idea of the size and consistency of the gland.
For more accurate and detailed measurements, particularly when a condition is suspected, imaging techniques like MRI are used.